A blood transfusion is when whole blood, or parts of the blood, are given to a person through an IV (intravenous) line placed in a vein. Whole blood or the parts of the blood used for transfusion are called blood products. The blood usually comes from another person. This person is called the donor.
Understanding blood and blood parts
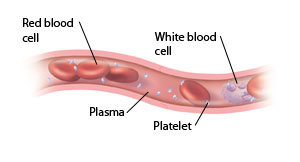
Blood is a fluid that flows throughout the body. It is made up of different parts that have specific roles.
-
Red blood cells (RBCs). They carry oxygen all over the body.
-
White blood cells (WBCs). They are part of the body’s immune system. Their main job is to help fight infections and diseases.
-
Platelets. These are fragments of blood cells that help with clotting. When you have a cut or bruise, platelets come together to form a clot or plug. This helps to control bleeding, so you don’t lose too much blood.
-
Plasma. This is the liquid base for whole blood. It carries the different types of blood cells to all parts of the body. Plasma also carries proteins called clotting factors. These help platelets with the clotting process.
Blood is divided into 4 types: A, B, AB, and O. Blood also has Rh types: positive (+) and negative (–). Any blood products you have during a transfusion must match your blood type.
Why a transfusion may be done
Cancer can cause problems that may need treatment with blood transfusions. For instance:
-
Cancer can affect the bone marrow. This is the soft, spongy part inside the bones where most of the body’s blood cells are made. When the bone marrow is damaged or destroyed, the body can't make enough blood cells. The body can't work normally without enough blood cells.
-
Cancer can cause anemia. This condition happens when there are too few red blood cells in the body. The body’s tissues and organs don't get enough oxygen without enough red blood cells. Anemia can make you feel tired or short of breath.
-
Sometimes certain cancers can cause internal bleeding. This can lead to blood loss that can threaten your health.
Certain treatments for cancer can lower the number of healthy blood cells in the body. A transfusion can help increase the number of healthy cells. These treatments include:
-
Chemotherapy (chemo). This uses strong medicines to help kill cancer cells. But these medicines can also damage healthy cells. This includes cells in the bone marrow. This can lower your blood cell counts.
-
Radiation. This uses strong X-rays to help kill cancer cells. Like chemo, this treatment can also damage healthy cells in the bone marrow. This can lower your blood cell counts.
-
Surgery. This may be needed to remove a group of cancerous cells, called a tumor, in the body. The surgery can cause blood loss and the need for transfusions.
Types of transfusions
Depending on what you need, your healthcare provider may advise 1 or more of the blood products listed below as part of your treatment plan. They will explain to you how the transfusions will be given and how often they may be needed. Before receiving any blood products, you may need to have some blood drawn. This is to identify your blood type and do an antibody screen. It is also done to test your blood against a donor's blood to make sure they are compatible (called crossmatching). You will also need to sign a consent form that says you understand the possible risks of having a transfusion.
RBC transfusions
These are most often used to treat severe anemia or blood loss. RBCs must match your blood type. Except in severe blood loss, people with cancer get RBCs without plasma. Each bag is called a unit. It takes about 2 to 4 hours to get 1 unit. During that time, nursing staff will be keeping track of your temperature, pulse, and blood pressure. They will also be watching for allergic reactions.
Platelet transfusions
These are used if your platelet count is too low. A low platelet count puts you at high risk of bleeding. Although it's best that platelets match your blood type, it is not needed. Platelets can be obtained in different ways:
-
From a donor (apheresis product)
-
Combined from several bags of whole blood (pooled product)
-
From a community donor who is specially matched (matched product)
It takes about 1 hour or less to get 1 unit of platelets. As with RBCs, nurses will keep track of your temperature, pulse, and blood pressure. They will be watching for allergic reactions.
Plasma (FFP) transfusions
These may be used to supply the blood with more clotting factors to help stop excess bleeding. Fresh frozen plasma (FFP) must match your blood type. One unit or bag of plasma is taken from a unit of whole blood. It is then frozen at the blood bank. Plasma is thawed when it is needed. It usually takes 1 to 2 hours to get 1 unit of FFP.
WBC (Granulocyte) transfusions
Due to the severe risks involved, these transfusions are rarely used. If there is a problem with the WBCs, your healthcare provider may suggest other treatments to help encourage the growth of new WBCs.
Whole blood transfusion
When a person needs all of the components in blood, whole blood is used. This type of transfusion is usually given to people with significant blood loss due to surgery or trauma.
Risks and possible complications of blood and blood product transfusions
These include the following:
-
Fever and chills
-
Allergic reaction, such as itchy skin or rash, trouble breathing, throat tightness, dizziness, redness, or flushing of the face
-
Chest pain
-
Low blood pressure
In the rare event of receiving the wrong blood type:
-
Back pain
-
Fast heart rate
-
Low blood pressure
-
Nausea
-
Dark or red pee
Although extremely rare, some diseases can be transmitted through blood transfusions. They include:
-
Hepatitis B
-
Hepatitis C
-
CMV (cytomegalovirus)
-
HIV
-
Bacterial infections