When Your Child Has a Cold or Flu
Updated for the 2025-2026 flu season
Colds and influenza (flu) infect the upper respiratory tract. This includes the mouth, nose, nasal passages, and throat. Both illnesses are caused by germs called viruses, and both share some of the same symptoms. But colds and the flu differ in a few key ways. Knowing more about these infections may make it easier to prevent them. And if your child does get sick, you can help keep symptoms from becoming worse.
What is a cold?
-
Symptoms include runny or stuffy nose, cough, sneezing, sore throat, and lower grade fevers. Cold symptoms tend to be milder than flu symptoms.
-
Cold symptoms come on slowly.
-
Children with a cold may be able to do many of their usual activities. They rarely complain of weakness or fatigue.
-
Symptoms may last up to 2 weeks.
What is the flu?
-
Influenza is a respiratory infection. (It’s not the same as the stomach flu, which is gastroenteritis: an inflammation of the lining of the stomach and intestines).
-
Symptoms include fever, headache, tiredness, cough, sore throat, runny nose, chest discomfort, and muscle or body aches. Children may also have an upset stomach and vomiting.
-
Flu symptoms tend to come on quickly.
-
Children with the flu may feel too worn out to do their normal activities.
-
Symptoms usually last 1-2 weeks.
How do colds and the flu spread?
The viruses that cause colds and the flu spread in droplets when someone who is sick coughs or sneezes. Children can breathe in the germs directly. But they can also pick up the virus by touching a surface where droplets have landed such as door knobs, toys, or countertops. Germs then enter a child’s body when they touch their eyes, nose, or mouth. Colds can also spread from direct contact with an infected person, such as by hugging or shaking hands. Colds are not caused by cold climates or being exposed to cold air.
Why do children get colds and the flu?
Children get colds and the flu more often than adults do. Here are some reasons why:
-
Less resistance. A child’s immune system is not as strong as an adult’s when it comes to fighting cold and flu germs.
-
Winter season. Most respiratory illnesses occur in fall and winter when children are indoors and exposed to more germs.
-
School or daycare. Colds and the flu spread easily when children are in close contact.
-
Hand-to-mouth contact. Children are likely to touch their eyes, nose, or mouth without washing their hands. This is the most common way germs spread.
How are colds and the flu diagnosed?
Most often, doctors diagnose a cold or the flu based on the child’s symptoms and a physical exam. Children may also have throat or nasal swabs to check for bacteria and viruses. Your child’s doctor may do other tests, depending on your child’s symptoms and overall health. These tests may include:
How are colds and the flu treated?
Most children recover from colds and the flu on their own. Antibiotics don't work against cold viruses, so they are not prescribed for them. Antiviral medicines can help shorten the symptoms of the flu. This is especially important if the child is at risk of or is developing complications of the flu. These medicines work best if they are started soon after your child shows symptoms.
For both illnesses, other treatments can help ease your child’s symptoms until your child recovers. To help your child feel better:
-
Give your child lots of fluids, such as water, electrolyte solutions, apple juice, and warm soup, to prevent fluid loss (dehydration).
-
Give a bland diet. Often children with colds or flu do better on a bland diet. It is made up of foods that are soft, not very spicy, and low in fiber. You may try:
-
Breads, crackers, and pasta made with refined white flour.
-
Refined hot cereals, such as oatmeal and Cream of Wheat.
-
Fruit juices that are diluted by mixing half water and half juice. Do not give your child too much fruit or apple juice.
-
Make sure your child gets plenty of rest.
-
Have older children gargle with warm saltwater if they have a sore throat. Do not give cough drops or lozenges if your child is younger than 4 years, as he or she could choke on them.
-
To ease nasal congestion, try saline nasal sprays. You can buy them without a prescription, and they’re safe for children. These are not the same as nasal decongestant sprays. Those sprays may make symptoms worse if overused.
-
Consider using a cool mist humidifier in your child's room. Humidified air may improve symptoms of nasal congestion and runny nose.
-
Clean the humidifier as frequently as recommended by the manufacturer to prevent the growth of mold and bacteria or build-up of minerals.
-
To manage fever, strictly follow your doctor's instructions about how much and how often you should give the fever medicine. Always check the instructions on the package. You may also follow these tips:
-
Don't bundle up your child with blankets or extra clothes, even if they have the chills. Try one layer of lightweight clothes and a lightweight blanket for sleep.
-
Your child's room should be comfortable, not too hot or too cool. Use a fan at low speed if the room is hot or stuffy.
-
Give a lukewarm bath or sponge bath to help cool the fever.
-
Don't use cold baths, ice, or alcohol rubs. These often cause shivering and make things worse.
-
Use children’s-strength medicine for symptoms. Discuss all over-the-counter (OTC) products, herbal and alternative treatments with your child’s doctor before using them. Note: Don’t give OTC cough and cold medicines to a child younger than 6 years old unless the doctor tells you to.
-
Do not give aspirin to children or teens unless your child’s doctor says it is safe. Aspirin can put your child at risk for Reye syndrome, a rare but serious condition.
-
Never give ibuprofen to an infant age 6 months or younger.
-
Keep your child home until they have been fever-free for 24 hours.
Preventing colds and the flu
To help children stay healthy:
-
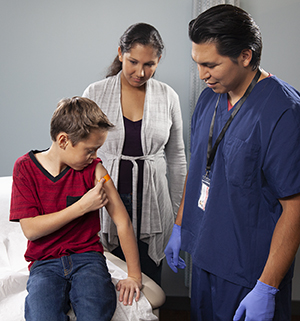
Get a flu vaccine for your child every year. A yearly flu vaccine is recommended for all children ages 6 months and older with few exceptions. The vaccine is often given as a shot. A nasal spray made of live but weakened flu virus may also be given. The nasal spray is for healthy children 2 years and older who don't get the flu shot. Because of COVID-19 and RSV, experts strongly advise getting a flu vaccine to protect yourself, your family, and others. Flu, COVID-19, and RSV viruses are all likely to spread during flu season. People at high risk for complications from the flu are also likely to be at high risk for serious problems, so it's important to get a flu vaccine.
-
Teach children to wash their hands often—before eating and after using the bathroom, playing with animals, or coughing or sneezing. Carry an alcohol-based hand gel (containing at least 60% alcohol) for times when soap and water aren’t available. Hand rubs should be spread over the entire surface of hands, fingers, and wrists until dry.
-
Remind children not to touch their eyes, nose, or mouth.
-
Consider having your child wear a medical mask when around others with colds or the flu. Medical mask use reduces the chance of coming down with these illnesses (in addition to reducing the risk of COVID-19).
-
Avoid people who are sick, when possible.
Tips for correct handwashing
Use clean, running water and plenty of soap. Work up a good lather.
-
Clean the whole hand, under the nails, between the fingers, and up the wrists.
-
Wash for at least 20 seconds (as long as it takes to say the alphabet or sing the Happy Birthday song). Don’t just wipe—scrub well.
-
Rinse well. Let the water run down the fingers, not up the wrists.
-
In a public restroom, use a paper towel to turn off the faucet and open the door.
When to contact your child’s doctor
Contact your child’s doctor if:
-
Your child doesn't get better.
-
Your child is short of breath or has fast breathing.
-
Thick, yellow- or green-colored discharge comes from the nose.
-
Thick yellow or green mucus comes up with coughing.
-
Your child has worsening symptoms, especially after a period of improvement.
-
Your child has a fever (see Fever and children, below).
-
Your child has severe or continued vomiting.
-
Your child shows signs of dehydration. They include a dry mouth, dark or strong-smelling urine or no urine output in 6 to 8 hours, no tears while crying, and refusal to drink fluids.
-
Your child has trouble waking up, or your child does not act alert or more comfortable when their fever goes down.
-
Your child has ear pain (ear pulling, fussiness in toddlers).
-
Your child has sinus pain or pressure.
If your child is younger than 2 years, contact their doctor before giving medicine. If your child is younger than 3 months and has a fever, contact their doctor immediately.
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The doctor may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The doctor may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel okay using a rectal thermometer, ask the doctor what type to use instead. When you talk with any health care provider about your child’s fever, tell them which type you used.
Below is when to contact the doctor if your child has a fever. Your child’s doctor may give you different numbers. Follow their instructions.
When to contact a doctor about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s doctor how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the doctor
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the doctor
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the doctor